Pancreatic cancer is one of the deadliest forms of cancer with most patients surviving much less than one year from diagnosis. This was certainly the experience that my family had—diagnosis was made at the end of January and the patient died in April. For patients with metastatic disease, combination therapy with conventional chemotherapeutic agents, which kill all rapidly dividing cells, is the only option. This treatment, which has severe side effects, typically only extends life at most a few months and can be intolerable if the patient’s health is already compromised by the cancer.
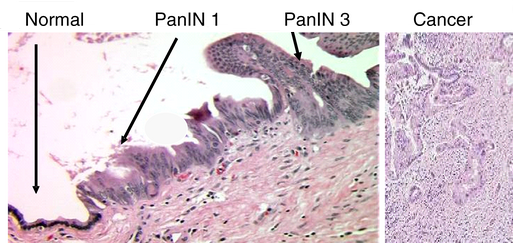
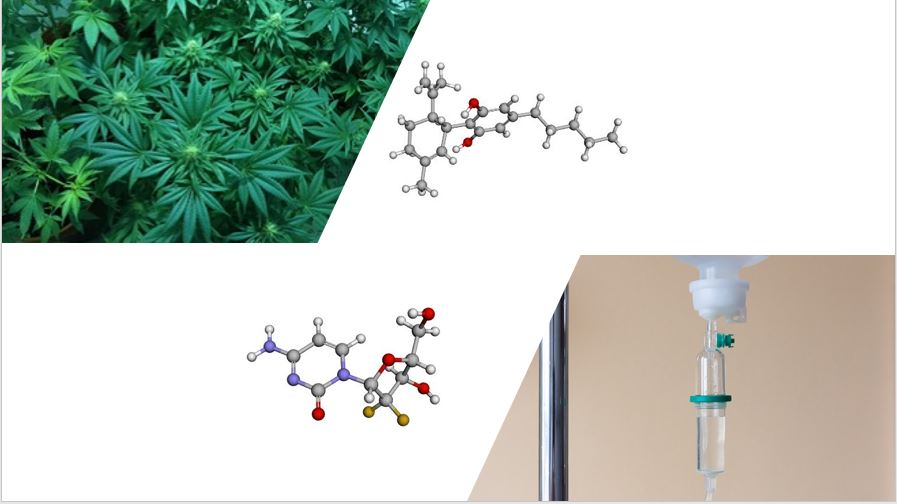
To research this deadly form of the disease called PDAC (pancreatic ductal adenocarcinoma), scientists use a mouse genetically engineered to spontaneously develop pancreatic cancer. This KPC mouse model has mutated forms of 2 genes that are also mutated in PDAC cells in patients, and the mice go through the same stages in disease progression as are observed in patients (Figure 1). The genes are TP53, which is missing or nonfunctional, and KRAS, which has an activating mutation. TP53 is a tumor suppressor, and KRAS is an oncogene.
Ferro and colleagues studied whether inhibition of a receptor called GPR55 would provide a synergistic (better than additive) benefit when combined with gemcitabine. Gemcitabine is a conventional chemotherapeutic, a nucleoside analog, that blocks DNA replication and thus impairs cell proliferation. GPR55 is a member of the G protein-coupled receptor (GPCR) family. Even though this the largest family of receptors in humans, there are relatively few drugs for cancer that target GPCRs. GPR55 is activated by a lipid called lysophosphatidylinositol. Of therapeutic relevance, this receptor has been implicated in colorectal cancer, breast cancer, and pancreatic cancer. GPR55 is inhibited by a cannabinoid compound called cannabidiol (CBD), one of the many bioactive compounds in marijuana (Figure 2). Unlike tetrahydrocannabinol (THC), CBD is not hallucinogenic. CBD interacts with different receptors than those for THC, and it has a different effect on the receptors that THC activates. CBD interacts with other receptors besides GPR55, but the work of Ferro and colleagues showed that GPR55 is the relevant receptor for this anti-cancer activity of CBD.
Studies with PDAC cells in culture showed that GPR55 stimulated cell division and anchorage-independent growth, a hallmark of malignant cells. Reducing the abundance of GPR55 reduced signaling through a growth-promoting pathway, called the MAPK pathway. CBD and another antagonist reduced cell proliferation and anchorage-independent growth.
GPR55 is present in healthy pancreas, but it is only found in the Islets of Langerhans where hormones are produced. GPR55 was abundant in ~25% of PDAC samples from patients. PDAC tumors arise in from ductal cells, which are not positive for GPR55 in healthy pancreas.
By breeding the KPC mice to mice lacking the gene encoding GPR55, Ferro and colleagues generated KPCG mice. Compared with the KPC mice, the KPCG mice survived longer, although not as long as wild-type mice. The pancreatic tumor cells were less proliferative in the KPCG mice, delaying the progression of the pancreatic cancer. Treating the KPC mice with CBD alone, gemcitabine alone, or CBD and gemcitabine showed that the combination treatment extended survival three time longer than mice not given any treatment (56 days for combined therapy versus 20 days without therapy and 22 or 23 days with single agent therapy).
This preclinical study provides encouraging support for continued research into the medical benefits of compounds present or derived from marijuana.
Highlighted Article
R. Ferro, A. Adamska, R. Lattanzio, I. Mavrommati, C. E. Edling, S. A. Arifin, C. A. Fyffe, G. Sala, L. Sacchetto, G. Chiorino, V. De Laurenzi, M. Piantelli, O. J. Sansom, T. Maffucci, M. Falasca, GPR55 signalling promotes proliferation of pancreatic cancer cells and tumour growth in mice, and its inhibition increases effects of gemcitabine. Oncogene 10.1038/s41388-018-0390-1 (30 July 2018). PubMed
Related Resources
Gemcitabine, Drugbank https://www.drugbank.ca/drugs/DB00441 (accessed 1 August 2018)
Cannabidiol, Drugbank https://www.drugbank.ca/drugs/DB09061 (accessed 1 August 2018)
GPR55, UniProt https://www.uniprot.org/uniprot/Q9Y2T6 (accessed 1 August 2018)
Pancreatic cancer information on Cancer.Net. ASCO. https://www.cancer.net/cancer-types/pancreatic-cancer/introduction (accessed on 1 August 2018)
Cite as: N. R. Gough, Cannabinoid combo therapy for pancreatic cancer. BioSerendipity (2 August 2018) https://www.bioserendipity.com/cannabinoid-combo-therapy/