Osteoarthritis is the form of arthritis that many people develop as they age. It is associated with breakdown of the cartilage in joints, causing pain and difficulty moving the affected joint. In contrast to rheumatoid arthritis, which is an autoimmune disease, osteoarthritis is thought to arise from mechanical wear and tear of the joint or in response to joint injury. Wang and colleagues present evidence that mast cells are involved in the damage to cartilage that occurs with osteoarthritis.
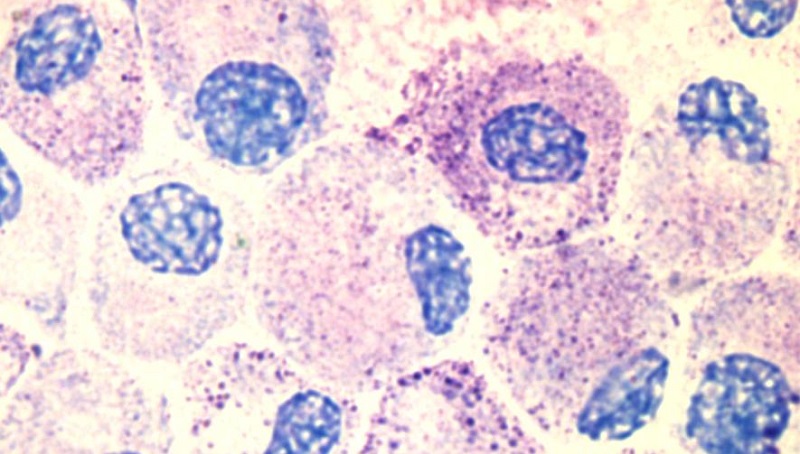
Mast cells are best known for their roles in allergies. When activated by the antibody IgE, mast cells release inflammatory mediators and enzymes through a process called degranulation. One of the enzymes is called tryptase. Wang and colleagues measured the amount of tryptase in the joint fluid of patients with osteoarthritis and patients without osteoarthritis but with an injured joint. Both joints had mast cells, but the osteoarthritic joints had higher amounts of tryptase and degranulated mast cells (those releasing their inflammatory and tissue-degrading contents).
To show that mast cells were important for symptoms of arthritis, the researchers used mice engineered so that they did not have functional mast cells. Both of these mouse strains were protected from developing experimentally induced osteoarthritis. Mice engineered to lack IgE or the receptor that IgE binds were also protected from osteoarthritis. Inhibiting tryptase with a drug, blocking IgE from activating its receptor on the mast cells, or inhibiting an enzyme needed for mast cell activation also protected the mice from experimentally induced osteoarthritis.
This study suggests that IgE-mediated activation of mast cells contributes to the pathological tissue remodeling that occurs in joints and causes osteoarthritis, at least in the form caused by injury. This study suggests new options for treating and potentially preventing tissue damage and the development of osteoarthritis. One of the reviewers noted that IgE is not increased in the circulation of patients with osteoarthritis and that it is not clear if there is a joint antigen (a specific molecule in the joints that the IgE antibody recognizes) involved. Future studies are needed to confirm in humans that the source of tryptase is mast cells and, if they are, that IgE is what stimulates these cells to degranulate.
Highlighted Article
Q. Wang, C. M. Lepus, H. Raghu, L. L. Reber, M. M. Tsai, H. H. Wong, E. von Kaeppler, N. Lingampalli, M. S. Bloom, N. Hu, E. E. Elliott, F. Oliviero, L. Punzi, N. J. Giori, S. B. Goodman, C. R. Chu, J. Sokolove, Y. Fukuoka, L.B. Schwartz, S. J. Galli, W. H. Robinson, IgE-mediated mast cell activation promotes inflammation and cartilage destruction in osteoarthritis. eLife 8, e39905 (2019) DOI: 10.7554/eLife.39905. PubMed
Cover image details
Also of interest…
Stem Cell Injections for Osteoarthritic Knees
Cite as: N. R. Gough, Beyond Allergies: Mast Cells Contribute to Osteoarthritis. BioSerendipity (1 June 2019) https://www.bioserendipity.com/mast-cells-contribute-to-osteoarthritis/